One of the most commonly performed tests in dry eye diagnosis is the Tear Break-Up Time test (aka TBUT). Here, we look the current test and reasons why there may be better, more modern and less intrusive methods to evaluate tear stability.
Why is Measuring Tear Stability Important?
Tear Break-Up Time tells us how well the tears stay coated on your eyes. When the tears break-up it means that small gaps start to appear in the tear film coating your eyes. Poor quality tears tend to break-up much quicker. When the tears break-up, it exposes the cornea to the atmosphere causing it to dry out. This ultimately causes damage to cells at the front of the cornea and conjunctiva often resulting in symptoms of discomfort and signs of drying and cell loss.
What Would the Best Tear Stability Test be Like?
The best tests for assessing tear film stability should not interfere with the tear film. In general, this means we don’t want a test that adds chemicals to the tears or causes reflex tearing, for example, from bright lights.
Tests that minimise any external influence on tear stability are non-invasive. Hence the name Non-Invasive Tear Break-Up Time (NIBUT),
As its name implies, tear break-up time assess the time it takes for the tears to ‘break-up’. Thererfore, the clinician performing the test usually measures the time he or she sees the tears breaking up. There are a number of issues with this approach:
- Break-up time only provides information of the tears breaking up at one point on the cornea. What about the rest of the cornea?
- Simple time based measurement is prone to significant variation within the same patient.
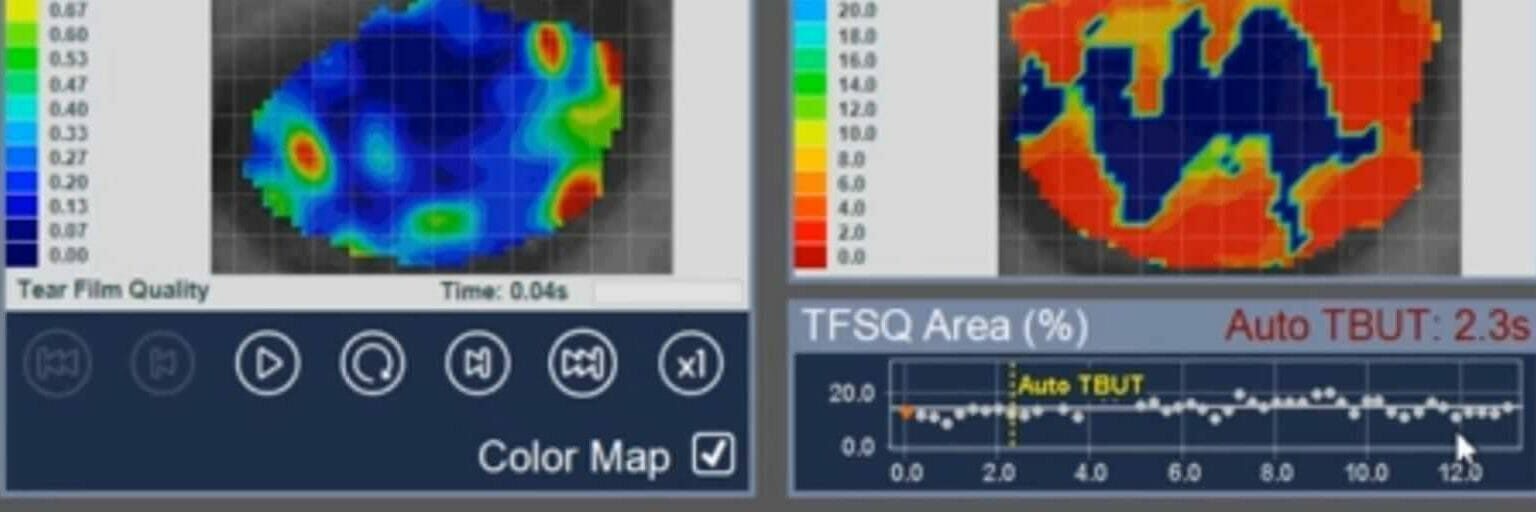
As a result of these issues, automated non-invasive tear break-up tests provide much improved repeatability and also precision in diagnosing dry eye disease. I’ll discuss one of these later, but first let’s see just how variable the standard fluorescein break-up time test is.
Fluorescein Break-Up Time (FBUT)
Fluorescein Break-Up Time or FBUT is the most commonly used method to assess the stability of the tears. It involves adding a dye (called Fluorescein) into the eye. The dye mixes with the tears and fluoresces green when blue light is shone on the eyes. When the tears are unstable and break-up, dark patches appear highlighting areas of tear break-up.
So, the problem with fluorescein break-up time is that it adds a foreign chemical to the tears which of course in itself cause the tears to become less stable. Secondly, it provides only a time based assessment on the break-up of tears. There’s no information on the surface quality of tears and because of the variability, it needs to be performe 3 times. Of course, there are other issues, for example, the amount of fluroescein added is never delivered consistently, so again leading more variability.
In fact, the literature states (Vitali et al, 1994) that the sensitivity of FBUT is 72.2% and specificity 61.6% which means that for every 100 positive results for dry eye, only 72.2 will truly have dry eye. The specificity indicates that for 100 people who don’t have dry eye, FBUT will indicate that 38.4 have dry eye. This is one of the reasons why no single test for dry eye is ever perfect. Clinicians use the results from multiple tests to come to a diagnosis. However, if the sensitivity and specificity of a test are high then the probability of a correct diagnosis is increased.
Automated Non-Invasive Tear Break-Up Time
Developments in corneal topography devices have led to improvements in the measurement of tear film stability. They eliminate teh need to add a
References
Vitali C, Moutsopoulos HM, Bombardieri S. The European Community StudyGroup on diagnostic criteria for Sj€ogren’s Syndrome. Sensitivity and speci-ficity of tests for ocular and oral involvement in Sjogren’s syndrome. AnnRheum Dis 1994;53:637e47.